The creation of a neo-vagina is one of the most important surgeries during the MTF medical transition.
There are three types of vaginoplasty:
– Penile Disassembly and Inversion Vaginoplasty (the most common in MTF sex reassignment)
– Intestinal Vaginoplasty (used for revision surgeries or when the patient presents with a penis of inadequate size)
– Non-Genital Flap (most often performed following oncological surgeries, infections, traumas, or when the MTF patient is not interested in having a vaginal cavity for penetrative intercourse)
For sex reassignment, vaginoplasty is usually performed in a single surgical procedure, which can be complemented with a second step to more extensively feminize the sexual organs.
Before surgery, all hairs must be removed from the patient’s penis and scrotum, which can take from three to six months.
The success of an MTF vaginoplasty depends on the creation of a natural-appearing vagina and mons pubis.

The surgery itself consists in the removal of the scrotum and the creation of the labia minora, labia majora, a sensitive neo-clitoris, and of a vaginal cavity of satisfying dimensions to enable penetrative intercourse.
Other elements may be considered—continuity of the labia majora, a damp appearance for the labia minora, natural lubrication of the vagina walls enabling fluidity in intercourse. The clitoral hood is also shaped, to make it natural in appearance and sensitive.
The surgeon uses the skin of the penis and a pedicle scrotal flap to create the vaginal cavity. The labia majora are created with the lateral part of the scrotum, and the neo-clitoris is constructed with the back part of the penis glans. The labia minora and the vestibular lining are built by transplanting tissue from the urethra and penis skin. The urethra is then shortened. Transplants from other donor sites, for example from the lower abdomen, may be required.
A second optional step, which includes the following, can be performed a minimum of three months after vaginoplasty:
– Labioplasty to shape the labia minora
– Clitoral hooding to improve the appearance of the neo-clitoris
Intestinal vaginoplasty
Advantages of intestinal vaginoplasty include the creation of a 12 to 15 cm vascularized and naturally lubricated vagina. This may make the use of a gel-type lubricant for intercourse unnecessary. And post-surgical dilation is much less demanding.
Disadvantages include a risk of excessive vaginal secretion. The vagina may also suffer from an unpleasant odor.
For these reasons intestinal vaginoplasty is more often used for corrections than to create the neo-vagina originally.
Non-genital flap
A non-genital flap is often created for genital reconstruction following trauma, oncological surgery, or serious infection. Such flaps are sometimes also used for MTF transsexuals who are not interested in having a vaginal tract that would enable penetrative intercourse. In this case, only the external female sex organs—clitoris, labia, mons pubis—are constructed.
Post-surgery
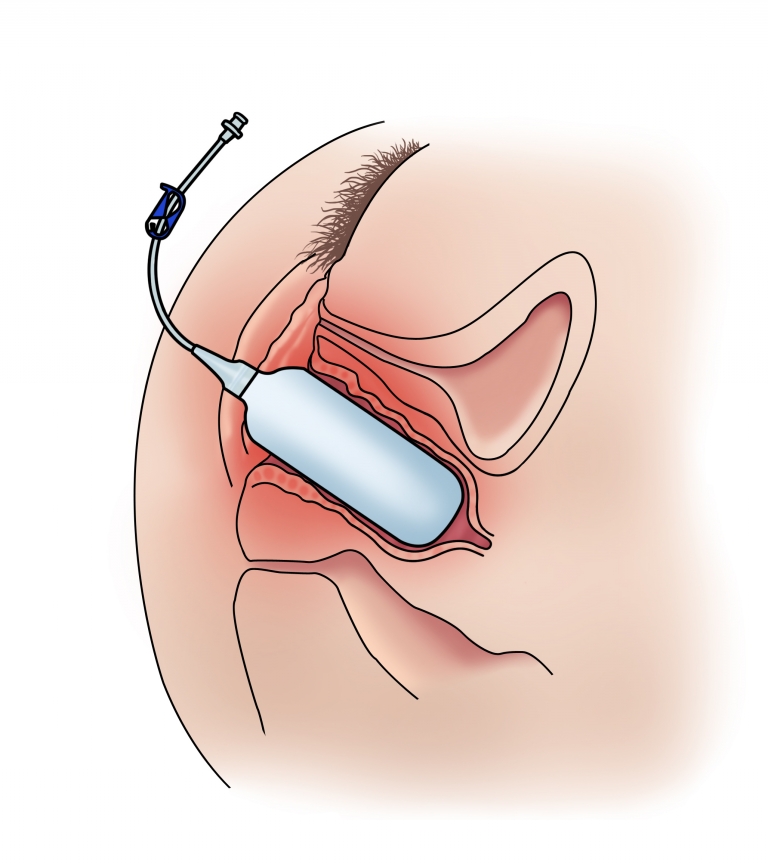
Four to five days of rest with a vaginal stent is required to let the inner walls settle and help promote micro-vascularization.
To avoid necrosis or the closing of the cavity, a vaginal dilator should be used several times a day for six weeks, after which its use can be reduced gradually to two or three times per week. The need for the use of a dilator also depends on the frequency of penetrative intercourse.

ZSI is the only European manufacturer of artificial urinary sphincters and of malleable and inflatable penile implants, as solutions for male urological problems (incontinence), sexual complications (Erectile Dysfunction), and gender identity procedures (prostheses for trans men and women).